Top 5 Drinking Water Issues To Be Resolved
By Joseph A. Cotruvo, PhD, BCES

These comments address five major current topics that U.S. EPA has on its agenda: the Lead and Copper Rule (LCR) proposal, perchlorate, per- and polyfluoroalkyl substances (PFAS), Legionella and water’s nexus to legionellosis, and distribution systems. The latter two, Legionella and distribution systems, provide the greatest public health risks associated with drinking water and warrant the highest priorities for management, investments, and health and safety improvements.
Lead and Copper Rule (LCR) Proposal
EPA issued a proposed revision of the LCR on 11/13/2019. The original LCR was promulgated in 1991. It differed from all previous regulations. A maximum contaminant level (MCL) was not feasible because of the unique origin of lead in drinking water at the tap, which is from the corrosive effect of metal surfaces that water contacted on the way to the tap, and thus the variability of conditions and effects in virtually each dwelling and building. Lead service lines (LSLs), old galvanized iron pipe in old residences, leaded brass faucets, and perhaps old (pre-1986) lead solders are the sources. The LCR was geared to determine whether the water being served by the supplier was excessively aggressive to those features to warrant corrective actions to reduce corrosion and lead releases. That determination is to be made using a virtual worst-case collection of a 1-liter first draw sample after sufficient stagnation. Monitoring sites were required to be weighted toward likely worst-case locations, such as likely presence of LSLs. Compliance was specified to begin with corrosion control, which, if inadequate, would require an LSL replacement schedule. The latter would be only a partial resolution, because old galvanized pipe in old housing is another important source. A study of high lead detections in Washington, D.C. showed a very high correlation with high iron, and that was consistent with old galvanized plumbing in the home. Trace water lead accumulates on the iron oxide coatings that develop. Thus, emphasis on adequate corrosion control is essential so as not to suspend the internal iron oxide deposits. Washington and others have successfully utilized phosphate addition as a very effective way to significantly reduce lead releases.
The LCR has been successful where it was implemented and enforced. Unfortunately, that has not always been the case in some states and water systems. Flint, MI, is a prime example where the LCR was not enforced, and further, the state regulator allowed the water supplier to make significant changes of water source and treatment without the routine measures to evaluate the consequences of the choices prior to implementation. Fortunately, although water lead increased in some homes, only a small temporary increase in blood lead occurred in a small percentage of children. That was likely because consumption was greatly limited when the water became so obviously contaminated by discoloration and taste from suspension of sediments. However, the most likely adverse health outcome was many cases of legionellosis and at least 12 deaths due to inhalation of microbe-contaminated water aerosols probably during showering.
Figure 1 shows the downward trend of child blood leads in Flint over about 11 years (2006-2016). Note the 2014-2016 period when the water problem occurred, and also 2008 and 2011.
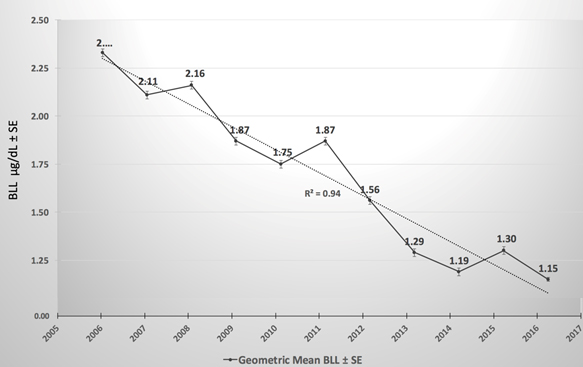
Figure 1. From Gomez et al.
There would not have been a lead problem in Flint if they had been in compliance with the LCR. So, the critical issue to be resolved is the best way to require the states to enforce and achieve universal compliance with the LCR, rather than establishing additional, potentially more confusing, regulatory requirements. The proposed new LCR is so complex that it raises more barriers to universal compliance as well as providing burdens that many, especially smaller water suppliers, would have serious difficulties understanding it, let alone complying with it.
Overall, there has been more than 95 percent reduction (from about 16 ug/dL to much less than 1 ug/dL) of average U.S. child blood lead since the 1976-1980 NHANES study prior to elimination of leaded gasoline. Old lead paint seems to be the cause of remaining high values. “Lead Reduction is a National Success Story” (Cotruvo, JA (2019). JAWWA April, 111:4, 73-75, 2019) describes several recommendations aimed at simplifying the existing LCR while facilitating the monitoring requirements, which are difficult to implement in their current form. Perhaps a good approach to facilitate removal of lead service lines would be legislation to include lead service and galvanized pipe mitigation as part of real estate transactions, like radon and lead paint mitigation that is often required. The cost would be buried in the sale price and effectively shared between the buyer and seller.
Perchlorate
EPA issued a proposal for regulation of perchlorate on June 26, 1919. Perchlorate can be present in water from some past industrial discharge and fertilizer activities, and some perchlorate can be generated by solar UV oxidation of chloride. Trace amounts can be present in aged hypochlorite disinfectant. Perchlorate binds with the sodium iodide symporter (NIS) that transports iodide to the thyroid, so excessive perchlorate can alter thyroid function in people who are not consuming sufficient dietary iodide. Poor thyroid performance can have adverse effects on neurological development of infants. EPA has an existing Health Advisory of 15 ppb, derived from a review by an earlier National Academy of Sciences expert panel. Some states have decided to use even lower concentration targets. The more recent World Health Organization (WHO) 2017 Guideline for perchlorate is 70 ppb. The EPA’s proposed options, including not to regulate, are reasonable for consideration and comment. The proposed middle option (56 ppb) is in the same ballpark and slightly lower than the 2017 WHO Guideline, so it can be considered to be reasonable for consideration of a possible regulation, if that course is decided. Few water supplies approach that concentration; however, a regulation also imposes monitoring costs.
Whether a national drinking water regulation for perchlorate would meet the Safe Drinking Water Act criteria for national regulation is open for debate. Some studies have concluded that regulation of perchlorate in drinking water would not meet a risk-cost-benefit test. EPA’s Inspector General issued a report in 2010 suggesting that rather than a drinking water regulation, the most beneficial public health approach would be to assure that all pregnant women received prenatal care that included iodine supplementation.
Per- and Polyfluoroalkyl Substances (PFAS)
Numerous perfluoro compounds have been produced and commercialized over the last 60 years, and they and many byproducts have entered the environment. Perfluorooctane sulfonic acid (PFOS) and perfluorooctanoic acid (PFOA) have received particular attention. These perfluoro compounds have numerous commercial uses because of their unusual chemical properties, such as in firefighting foams and water-repellant fabric coatings. They are being detected at low concentrations in a small percent of particularly groundwater supplies at parts-per-trillion levels, and especially associated with past uses of firefighting foams at airports and airbases, and some industrial point sources. The problem is that they are persistent and not subject to significant chemical or biodegradation in the environment, so once present they will not disappear for many years. PFOS and PFOA have been phased out in the U.S. as of 2006. Blood detections in the population have declined significantly from virtually 100 percent incidence since then, but existing groundwater contamination is persistent.
The challenge is to determine a rational toxicological basis for acceptable levels in drinking water, as well as for exposures from the other sources. There is considerable controversy on those acceptable levels. EPA has published Health Advisories of 70 ppt for combined PFOS and PFOA. The Canadian Guidelines are 600 ppt for PFOS and 200 ppt for PFOA. The Australian expert committee reviewing several high-exposure occupational epidemiological studies concluded: “There is mostly limited or no evidence for any link with human disease from these observed (exposure) differences”. Several states have adopted guidance or standard values in the ppt teens or as low as 5 ppt (1 ppt is 1 millionth of a ppm). Prior to any drinking water regulatory action, there is need for a mainstream scientific consensus on the appropriate “safe” levels for perfluorocompounds in water, as well as for other exposures, and the relative source contributions. Prior to further action, EPA should initiate an international process, perhaps with WHO, to provide credible consensus recommendations. That would overcome the multiplicity of values being applied, which confuses the public and undermines the credibility of risk assessment and regulatory processes. (https://news.bloombergenvironment.com/environment-and-energy/insight-we-need-scientifically-credible-health-benchmarks-for-pfas)
Legionella
Legionellosis is now the most significant waterborne disease in the U.S., and it is the only recent one that causes deaths. It is caused by inhalation of water aerosols, not by ingestion. Legionellosis and Pontiac Fever are caused by inhaling a sufficient dose of the bacteria, usually Legionella pneumophila or Legionella longbeachea, respectively. Figure 2 illustrates the increasing trend of legionellosis outbreaks and the reduced trend of traditional waterborne disease outbreaks since 1980. CDC now estimates about 70,000 annual cases of legionellosis and about 10 percent are fatal; most have a water nexus in some form.
Legionellosis is underreported because many pneumonia cases are not typed to identify the specific microorganism cause. Pontiac Fever has flu-like symptoms and is generally self-limiting and not fatal, so it is often not diagnosed or treated by a physician. Legionella bacteria grow primarily in warm-water environments such as building plumbing systems, cooling towers, spas and hot tubs, ornamental fountains, and wastewater oxidation and aeration basins. Cases generally increase in summer months. The optimal growth temperatures are in the range of +/-~25 to 50 degrees centigrade (~77 to 122 F), but they will grow outside of that range. They multiply in biofilms and in some amoebas that provide protein nutrients and also protect them from disinfectants.
The public at highest risk due to individual susceptibilities are the elderly, smokers, and the immune-compromised, including cancer patients. Many cases have occurred in hospital intensive-care units, long-term care facilities, hotels and spas, from building plumbing, and downwind from cooling towers and wastewater treatment facilities. However, cases have occurred in all age groups. The growing immunosuppressed population is at particular risk.
Any mitigation process for Legionella and legionellosis risk should be associated with the development, application, and periodic revision of a comprehensive water safety or management plan that incorporates a Hazard Assessment Critical Control Point (HAACP)-type management system for maintaining improved changes in building water-system conditions. These can include: (1) temperature management in hot water systems, (2) disinfection treatment — especially of warm and hot waters, but also cold water, (3) continuous presence of residual disinfectants to the water tap/outlet, (4) periodic surveillance and monitoring to detect changing Legionella presence, and (5) verification and regular iterations of effective practices.
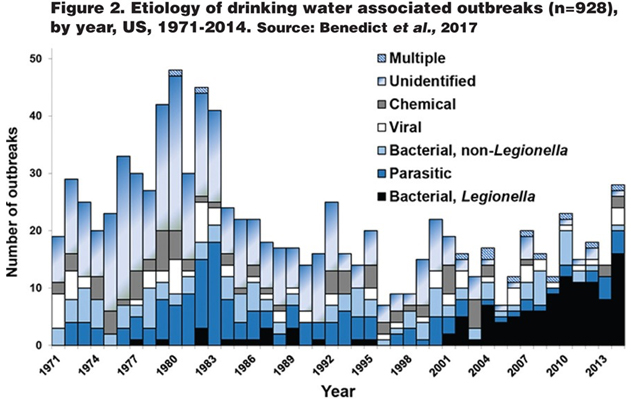
The CDC Morbidity and Mortality Weekly Report (MMWR) (2015) demonstrates that water-related Legionnaires’ disease is now the most significant waterborne disease in the U.S., and probably in other developed nations. Twenty-four of the 42 reported U.S. drinking water-associated outbreaks were caused by Legionella, resulting in 130 cases and 13 deaths; notably, it was the only cause of deaths among the reported waterborne outbreaks. MMWRs from the last decade indicate that about 60 percent of waterborne disease outbreaks and all deaths are due to legionellosis. Unpublished data from 2015 to 2017 in CDC’s National Outbreak Reporting System (NORS) indicated 89 drinking-water-related legionellosis outbreaks with 572 cases and 58 deaths.
Existing EPA drinking water regulation interpretations actually act as an impediment for hospitals to install supplemental disinfection to reduce risks to patients. They require that if any facility having more than 25 users adds treatment to the public water entering the facility, it becomes a public water system. Thus, a facility (e.g., building or hospital) that adds water treatment to water from a public water system would become a consecutive water system. That designation adds unfamiliar additional responsibilities and could adversely impact decisions on adding supplemental disinfection in their plumbing systems. Other countries, like Canada, the UK, and Australia, do not have similar requirements. The positive benefit-risk balance for a more appropriate interpretation is obvious. A different interpretation by EPA would facilitate actions that would immediately reduce legionellosis risks in those facilities. This could be done by variance and exemption guidance and would not require a regulatory change. (See: Cotruvo, JA. “Facilitating Supplemental Disinfection for Legionella Control in Plumbing Systems”. JAWWA. 106:8, 74-83, August 2014.)
Distribution System Degradation
Distribution systems are almost uniformly in various states of disrepair. Good-quality treated water leaving the water plant passes through aging distribution pipes, often coated with tuberculation and biofilms resulting in opportunities for reduced water quality. It has been estimated that about 500,000 water main breaks occur each year in the U.S. Not only do these require emergency repairs, and unbilled water loss, but they allow recontamination and seeding of distributed water by the likes of Legionella and other pathogenic microorganisms. The photomicrograph below illustrates the not-unusual interior condition of many distribution pipes, including encrustations and even rod-shaped bacteria.
Distribution systems probably constitute the major financial investment in water systems, and the greatest vulnerability for degradation of post-treatment water quality. Figure 2, above, shows the increase in distribution-related disease outbreaks versus source-related outbreaks that are well managed by filtration and disinfection. Many systems with piping well over 100 years old are currently in use and many water suppliers do not have aggressive programs for leak detection and reasonably rapid upgrades, because of costs. Water suppliers need to allocate dedicated funds to manage and restore their distribution systems to reduce the probability of breaks. 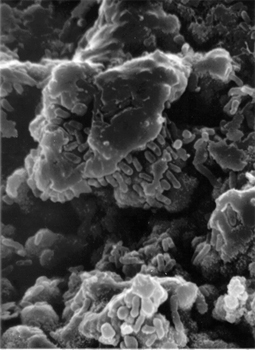
(See: “Drinking Water and Public Health in an Era of Aging Distribution Infrastructure”. Martin J. Allen, Neil Grigg, Robert Clark, Joseph Cotruvo. Public Works Management and Policy. October, 2018.)
Conclusion
This information summary provides factual information and suggestions regarding five topics of current interest in drinking water management. Legionella contamination and related distribution system replacement and repair constitute the greatest challenges to maintaining safe drinking water in the U.S. Addressing those two problems should be the highest priority for continued health protection by water suppliers and state and federal drinking water programs.
Joe Cotruvo was Director of U.S. EPA’s Drinking Water Standards Division after passage of the Safe Drinking Water Act. He is a member of the World Health Organization’s group that develops the series of WHO Guidelines for Drinking Water Quality, and is President of Joseph Cotruvo & Associates LLC, Water, Environment and Public Health Consultants, Washington, D.C.
